Chronic pain is defined as any pain that lasts for more than three months. When people experience chronic pain for a long period of time, it can lead to a downward spiral. As a result of the pain, you might become more inactive and sedentary, and your health may begin to deteriorate.
Physical therapists can help you manage your pain. Increasing the use of physical therapy could even make a real impact on the tragic levels of drug abuse that often begin with a prescription for pain medication. Living with chronic pain can be extremely difficult. But physical therapy is a crucial solution that can ease and even solve certain pains and reduce your overall pain level.
More Than Simply Hurting
Chronic pain affects each person differently. The good news is that physical therapy is not a one-size-fits-all approach to pain relief. Your physical therapist has many tools and techniques at their disposal to help alleviate and conquer chronic pain.
Chronic pain has a number of symptoms associated with it. Here are some of the associated symptoms of chronic aches and pains:
- Weight Gain: People with chronic pain may put on extra weight, which can lead to a host of added problems, from diabetes to heart disease.
- Activity Avoidance: People with chronic pain become fearful of normal activities. The fear of additional pain can cause people to withdraw from normal physical activities that they enjoy.
- Stiffness: Muscles and joints may feel stiffer when suffering from chronic pain.
- Reduced Fitness: Inactivity due to chronic pain can cause your muscles to weaken and shrink. This can have profound physical effects over time, even effecting your ability to balance.
- Reduced Circulation: Remaining inactive due to chronic pain reduces your circulation, which means your cells are not receiving a healthy amount of blood and oxygen. This can cause tissues to degenerate and lead to feelings of constant fatigue.
This dog has great balance. She must have gone to physical therapy.
What To Do If Pain Persists
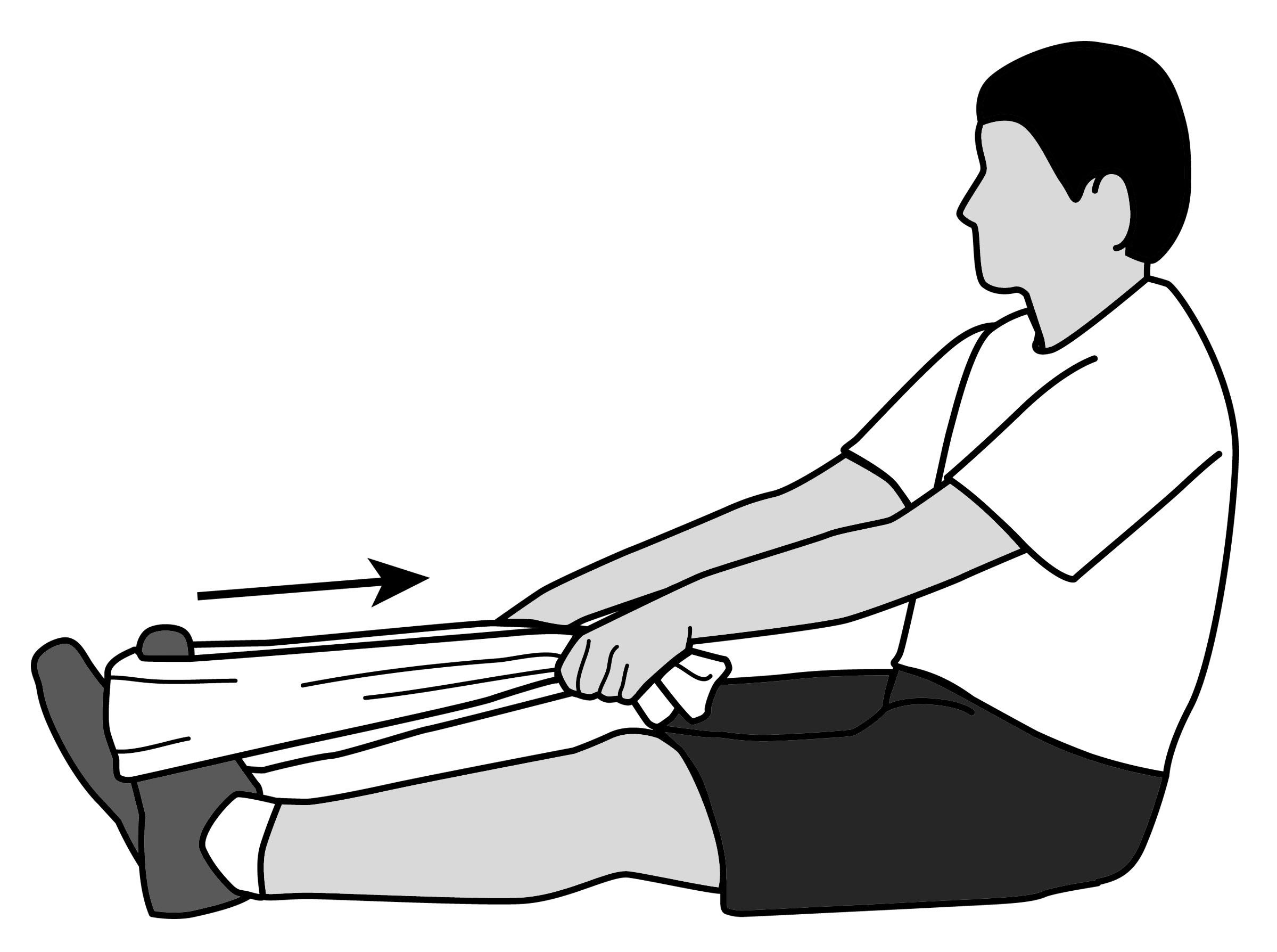
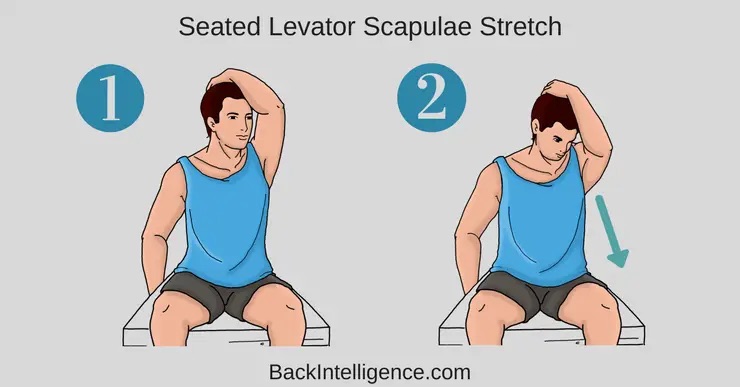
Your physical therapist will work with you to educate you on how to live a healthier lifestyle in order to keep aches and pains at bay. This can include anything from tips on staying hydrated and eating healthier to exercises and stretches you can do at home. The goal is to get you to the point where you are motivated to stay healthy without needing to go to physical therapy on a regular basis. All of this will help to alleviate your aches and pains.
Tom recommends physical therapy.
Physical therapy treatments will also include exercises, stretching, and flexibility. Over time, you will become stronger and more flexible, allowing you to move around more freely and with less pain. Your exercises will be designed to steadily improve your strength and flexibility. With a variety of tools available to treat and train you, we can make a big impact on your pain. Don’t hesitate to call and set up an appointment and get help.