When you have chronic pain, you tend to have a hard time getting a good night’s sleep. Pain and discomfort can distract you from falling asleep or keep you from falling into a deep sleep, when every little movement causes a flare-up with your pain. If you struggle with hip pain, then you may have difficulty finding a comfortable position to rest in because of the pressure and strain on your hip joints. When you are unable to sleep well, it can also make it difficult to heal after an injury or condition that is hurting you.
What Causes It?
Sciatica
The sciatic nerve is located at the base of your spine and travels throughout your hips, buttocks, and legs. When the sciatic nerve is aggravated or injured, it can cause a specific type of discomfort and pain in your lower back and lower half of your body known as sciatica. Some causes of sciatica are caused by a herniated disc in your lower back or spinal stenosis. You may notice that certain movements or positions can make the pain worse. Common symptoms of sciatica pain include tingling, weakness, and numbness, most commonly in just one of your legs.
Tendonitis
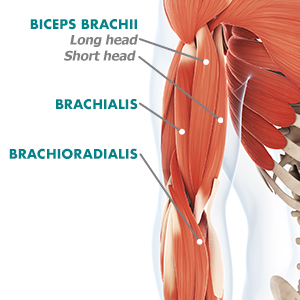
This refers to inflammation that affects tendons that connect muscle and bone. If you develop inflammation of a tendon in your hip, you might experience pain and discomfort with even the smallest of movements. Irritation and inflammation of tendons can lead to muscle tightness, tenderness, pain, and weakness in the area. Tendinitis is common in people who do sports with repetitive hip and leg movements, like running, swimming, and cycling.
Hip Bursitis
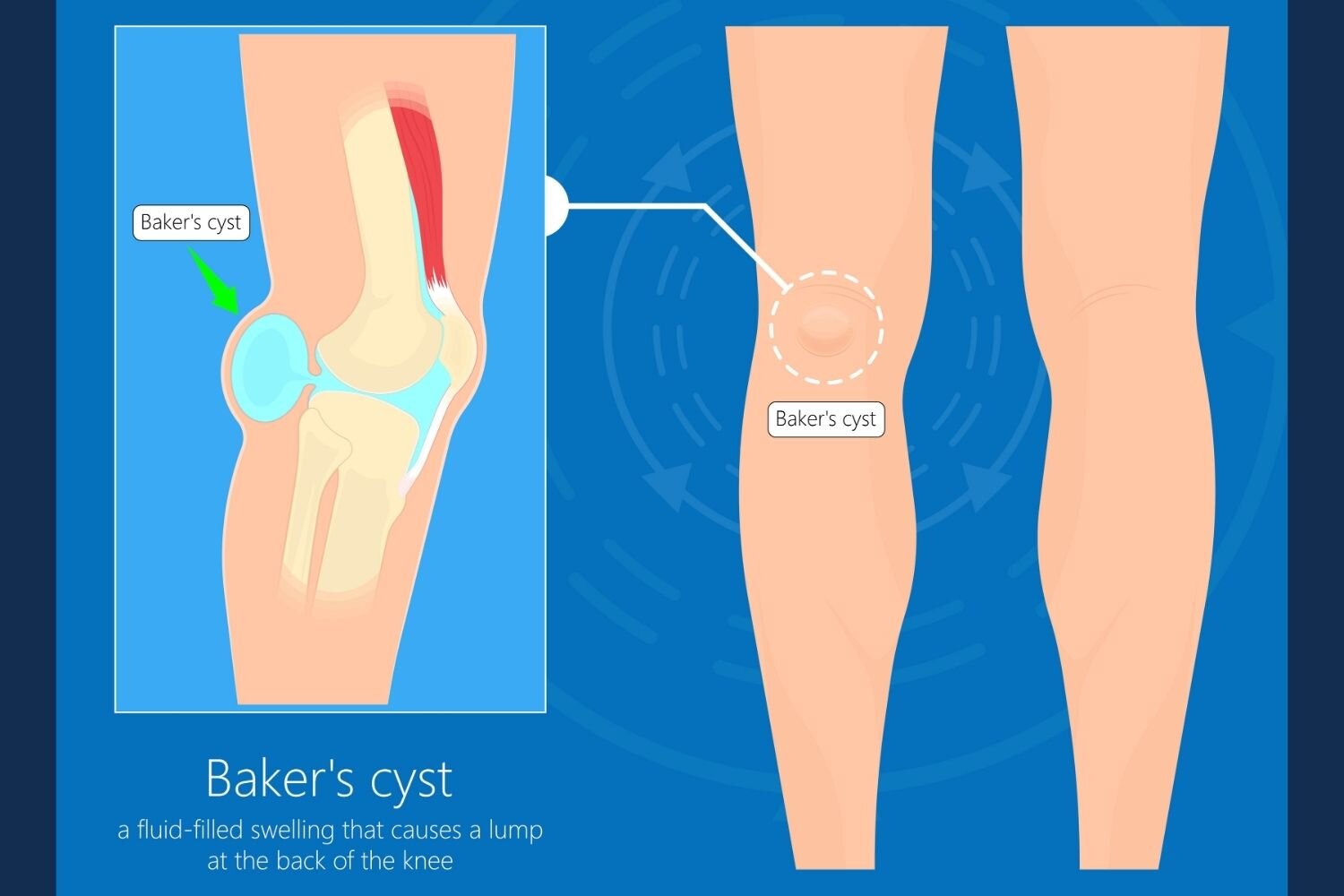
All of your joints have fluid-filled sacs that offer support to your joints. These fluid-filled sacs are known as bursae and if one of these becomes inflamed in your hip joint, then you might be diagnosed with hip bursitis. This condition is most often caused by repetitive movements that put strain and stress on the joints, leading to inflammation. If you have hip bursitis, your hip may feel achy and stiff, and you might feel pain with certain movements. Hip bursitis can also lead to sharp, shooting pains and swelling and redness in the area.
What to Do At Home
If you experience hip pain when sleeping, the first thing you might try to do is readjust your sleeping position.
Sleep on Your Side
One side may be more comfortable than the other, but side sleeping is a great position for relieving sciatica pain. You can even use pillows to help keep a natural separation between your knees and better support your lower back.
Try Sleeping on Your Back
Sleeping on your back might work best for you, but it may require a bit of trial and error. Try putting a pillow (or two) under your knees to relieve some pain. If that doesn’t work or you’re still uncomfortable, try a pillow or rolled-up towel under your lower back too.
Use Some Extra Pillows
Sometimes a pillow between your knees or under your back can make all the difference. You might want a body pillow or several extra pillows to help you get even more comfortable and maintain your pain-free position throughout the night.
You can also try taking a warm bath or icing the area before going to bed. This can help reduce inflammation in the area while also providing some pain relief. Also be sure to follow good sleep habits, like reducing screen time before bed, avoiding caffeine, and keeping your room at a good temperature. Additionally, you should ask your physical therapist about helpful stretches and exercises to try before bed that can help stretch out muscles that have gotten tight and stiff.
How can we help?
Our physical therapists can help provide you with tips and tricks to relieve hip pain while you sleep. This may include stretches and exercises to improve your strength and flexibility in that area. The supportive muscles, tendons, and other soft tissues that support your hip joint need to be strong and flexible in order to work properly and not cause pain. Your physical therapist can also teach you about foam rollers as well as stretches and exercises to do before and after workouts. Performing certain movements and stretches can also reduce pain if you sit or stand for long periods of time at your job.
If you are suffering from pain in your hips and it’s keeping you up at night, come in and see us at one of our offices. We can get you back to sawing logs in peace.