Good Posture
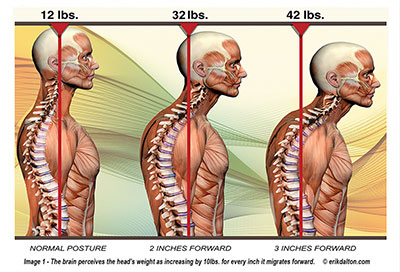
Good posture isn’t just for taking pictures with your family, there are real impacts to overall health that result from hunching shoulders. Our lives day to day shape our posture. Allowing bad posture to happen makes it more difficult to fix. Over time, if you keep your shoulders hunched your muscles will become trained to think hunched shoulders and a bent neck are natural.
A Life That Leads to Hunch
Looking at our phones and sitting at a computer has become a major part of all of our lives. Unfortunately, both of these encourage really poor posture. Often, hunched shoulders develop unconsciously through a few different ways. It could be unsupportive chairs, frequently carrying heavy objects, or avoiding attention in uncomfortable situations. Hunched shoulders negatively impact your appearance and body language. It also creates stress and pain in your neck, shoulders, and upper back. If left untreated poor posture can lead to chronic pain, fatigue and even difficulty breathing.
Diagnosis
Our physical therapists can judge if you have hunched shoulders and how severely. There are also simple tests you can do at home that can show if you have hunched shoulders. An easy way to check is to have a family member or friend look at your posture. One indicator is if you appear to be slouching even if you try standing up straight. Another sign is if the palms of your hands face behind you when you are standing at rest. With normal posture your thumbs face forward, and your palms face inward but hunched shoulders will force your thumbs to point inward and your palms to face back.
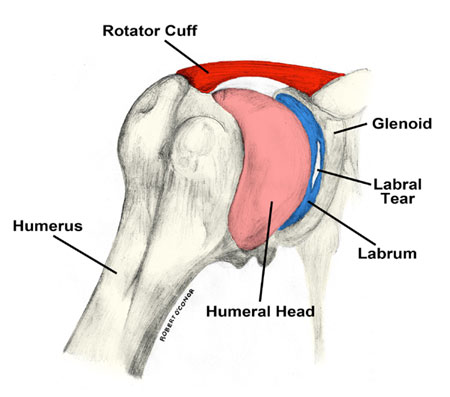
If you are experiencing low back, neck or shoulder pain, a physical therapist will be able to assess your posture and determine the source of your discomfort. If you are experiencing posture related symptoms, a physical therapist can develop personalized treatment plan aimed at correcting the corresponding weakness. Hunched shoulders could be a sign of more complicated weaknesses or dysfunction as well so it’s important to speak with a medical professional as soon as possible.
Treatment and Exercise
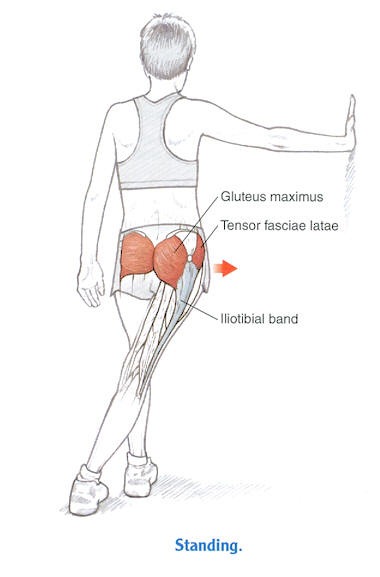
There are ways to treat and prevent hunched shoulders. A physical therapist will provide you with a unique exercise and stretch routine to address weaknesses or dysfunctions discovered during your initial evaluation. Just as the muscles and joints had learned to hold poor posture at rest, they can be strengthened and trained to hold good posture.
Stretches at Home
Handclasp
The handclasp stretch is simple and can be done every day. Standing up straight with your hands by your sides, reach your hands behind you to clasp them together.
Gently, pull your shoulders back, while being careful not to allow your neck to push forward.
Your shoulders should be pulled back until your chest opens and a deep stretch is felt. The position should be held for 30 seconds.
Shoulder Blade Squeeze
This basic exercise reminds your body what good posture feels like and helps build strength throughout the day.
Sitting up tall, you should move both of your shoulder blades together, as if trying to hold a tennis ball between them. As they flex, your shoulders should move down and away from your ears.
This position should be held for 10 seconds and repeated 10 times.
Come and See Us
There are many more stretches to be done at the physical therapy office and at home. Come see our expert therapists who will teach you the stretches and exercises that will be most beneficial for your condition. We will get you standing upright and in family picture shape in no time.